Opioid Abuse Intervention in Mid-Island, Staten Island
Scope of the Problem
In 2015, it was estimated that 33,000 deaths in the US were due to opioids, including prescription opioids, heroin and fentanyl. Additionally, in 2015, it was estimated that 2 million Americans had a substance abuse disorder from the use of prescription opioids, referred to as an opioid epidemic. Since 1999, the sale of prescription opioid drugs has almost quadrupled in the US. Staten Island has been affected by the epidemic on a large scale as well. Between 2015 and 2016, the number of deaths rose from 69 to 116, a 68% increase. In 2016, Staten Island had the highest overdose rate in New York City which surpassed even some of the worst affected US states. A recent study has shown that the epidemic is not confined to affluent young white residents, but affects all neighborhoods, races, socioeconomic backgrounds and ages, median age of overdose being around 37. Staten Island contains areas with the most overdoses but is the most underserved in terms of opioid addiction treatment clinics. There are only 2 methadone providers on Staten Island and 3 inpatient clinics, but only one of them offers detox services. After interviewing Staten Island residents, overprescription was found to be the main cause for opioid crisis, in addition to stigma, mental health comorbidity, boredom and fentanyl-laced heroin use.
Staten Island is roughly divided into 3 regions, the North Shore, Mid-Island, and South Shore. According to NYPD and the Richmond County District Attorney’s Office, Mid-Island has been identified as a high-occurrence area for opioid-related overdose and has been overlooked, according to the interviewed SI residents. Staten Island does have some public health programs that have been helping. There are programs for police officers and justice officials such as Naloxone training and usage and heroin overdose prevention and education program. Aftercare programs have also been successful, providing a range of activities after an individual has returned home from rehabilitation services. The SIHope website provides a one-stop place for drug users, family members and residents where they can find any pertinent information and treatment option. However, increase in facilities whose main focus is opioid abuse as well as a more educated SI community can aid in decreasing the Staten Island opioid crisis.
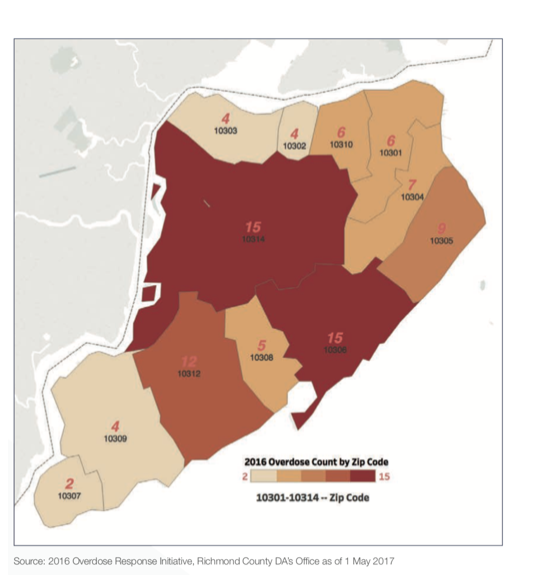
2016 Overdose Count by Zip Code
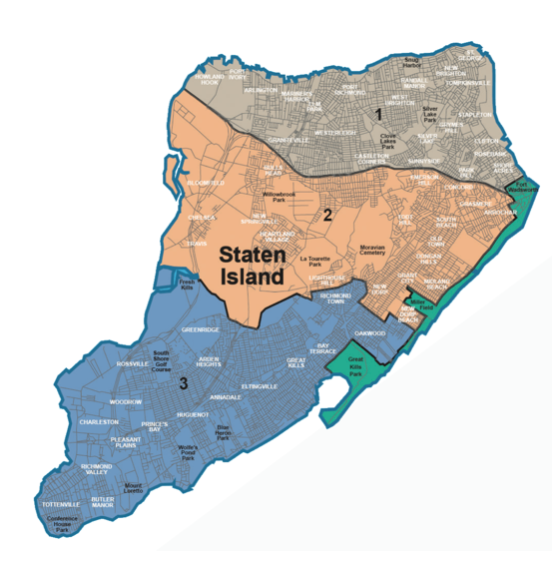
3 Regions of Staten Island: North Shore, Mid-Island, and South Shore
Planning
Possible interventions include both environmental and behavioral changes. Expansion of medication-assisted treatment options and inpatient detox clinics. Additionally, a targeted social campaign to educate Staten Island Mid-Island community about opioid addiction, reducing the stigma, addressing inaccurate misconceptions, and increasing awareness between family and friends.
Since there are few outpatient medication-assisted treatment or inpatient clinics to begin with, and they are already clustered in the North Shore of SI, additional facilities should be opened in the Mid-Island region where the number of overdoses is the highest. My key stakeholders include the Richmond Country district attorney, borough president, Staten Island University Hospital and SIUH Methadone Clinic, Richmond University Medical Center, Methadone Maintenance Treatment Program Clinic, representatives from the community and voluntary sectors, healthcare providers, patients, recovering addicts, family members, community pharmacies, residents of Mid-Island area and other SI elected officials.
Since I already have the data from NYPD and the Richmond County District Attorney’s Office on the number of opioid overdoses, and the 2017 report from the Columbia University School of International and Public Affairs on which SI individuals are affected, my next step would be to conduct a survey on what Mid-Island residents think about inpatient and outpatient clinics opening in their neighborhoods. The survey will be mailed and advertised on SI local news outlets. The survey will outline key facts about the opioid epidemic in SI and the lack of resources such as clinics in the Mid-Island area. I would then gather data from the inpatient and outpatient clinics that are currently open, on how much money they spend, how many people they treat, etc. My ultimate goal would be to reach out to SI elected officials with this data, such as the Richmond County District Attorney. Since the opioid epidemic is booming in SI, they would want to improve the problem as soon as possible.
For the targeted social campaign, I will attempt to utilize narrative stories of opioid overdose survivors, past opioid abusers, as well as family and friends of those who abuse/abused opioids. This social media campaign will solely focus on SI residents and will be relatable and personalized. Social media platforms will be utilized such as Facebook, Twitter and Instagram, and will be monitored by mediators who will be able to direct individuals toward available services and will make sure that there is no ill use such as online harassment. The campaign’s message toward individuals who are using opioids would be on stigma reduction, diversity of addiction and who it affects, what resources are available and how to access them. The campaign’s message toward family and friends of opioids users would also include that information but will also address symptoms of opioid addiction, how to react to these symptoms, any resources that are available and how to access them.
In order for the public health program to be funded, I would apply for funding from New York City. I would also encourage volunteer participation, especially among those who have been personally affected by the epidemic in some way. In order to aid in funding of social media campaign, I would seek out social media-focused adverting organizations that would either do the work pro-bono or offer any discounts. Staten Island high school and college students can also participate, which will count toward their volunteer hours and they will also be exposed to the information on the dangers of opioid misuse.
The program will be feasible in the long run since this is a growing epidemic and if something isn’t done soon, things will only get worse because addiction doesn’t just go away by itself. Staten Island officials and residents are already aware of the growing problem and any additional improvement to public health interventions will be welcomed. Unless drugs stop being addictive, I would expect this public health program to be useful in the long-run.
Development & Dissemination of the Intervention
The goal of this program is to increase access to inpatient and outpatient clinics in the Mid-Island region where opioid overdose is high and the access to such clinics is low. A social media campaign will also educate residents about opioid addiction, what symptoms to look for and how to handle them, address any misconceptions, and reduce the stigma of addiction so that opioid users will not be ashamed to seek help and the family/friends will not be ashamed to recognize abuse in their loved ones and aid them in getting help.
While the social media aspect of the intervention does not require a lot, opening additional clinics could be challenging. Since there is already data collected that will help support this intervention, additional data should be collected and analyzed from current open clinics as well as surveys addressing the opinions of SI residents. Collecting the data and analyzing it could take some time, but it should not be challenging. Volunteers could be used to gather data and trained individuals will analyze the data and come up with a proposed plan on why more clinics should be open. Since this issue is referred to as an epidemic, and the Columbia University School of international and Public Affairs has released a report of their assessment just last year, it is a time-pressing issue that needs to be improved. This proposed plan can be discussed with Michael McMahon first, district attorney for Richmond County who has announced the SI Hope program. We can also reach out to other SI elected officials that have expressed interests in curbing the opioid epidemic. This public health intervention does not require a lot of physical space. The survey will be mailed to SI residents, mentioned in the SI Live newspaper or other SI news outlets. SI Hope already offers the option where residents can request a yard sign to raise awareness.
Social media campaign does not require any physical space and very little funding. People would want to share their narrative experiences and will have an option to either go fully public or remain behind the scenes, sharing their story but staying anonymous. Mediators will make sure to address any questions, direct individuals toward available resources, and will make sure that social media comments do not get out of hand.
Evaluation & Maintenance
As it might take some time for the clinics to open, change may not be evident immediately. However, I believe it can be accessed yearly, based on opioid overdose deaths by each region of SI. If there has been a decrease and the outpatient and inpatient clinics report treating many patients, this public health intervention can be branched out to the North and South Shores. Social media campaign can be evaluated by how many individuals participated in the conversation and how many times the topic was shared on social media platforms by others overall. An additional post on social media can ask individuals whether or not they found social media campaign useful, which can be assessed every couple of months, where participants can express their opinions on what can be done to make it better. The program will continue to be publicly funded and will accept donations from anyone that wishes to help. The program will also have the support of SI residents as well as SI elected officials, which will help in its maintenance and longevity.
Sources:
https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.htm
https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief74.pdf
https://www.dnainfo.com/new-york/20170920/south-beach/columbia-university-opioid-study
http://www.snpnyc.org/wp-content/uploads/2017/09/CU-SIPA-Opioid-Capstone-2017.pdf



